High Velocity Therapy in Critical Care
A More Comfortable Way to Rehabilitate.
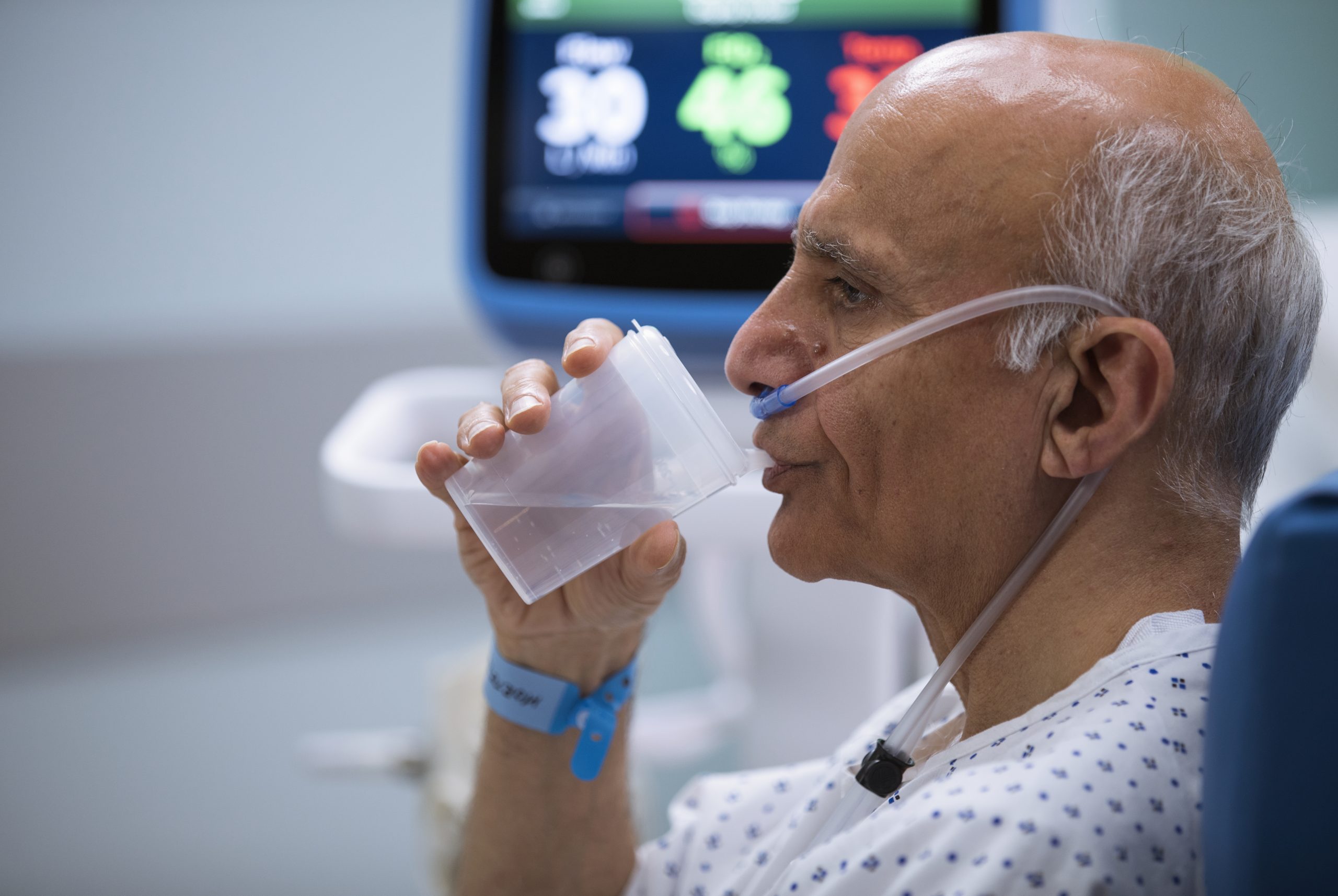
Never Compromise Comfort In Search of Efficiency
With high velocity therapy, you can offer patients in respiratory distress an attractive alternative to NiPPV for spontaneously breathing patients.
Vapotherm high velocity therapy offers the respiratory support patients in respiratory distress need, with the comfort and simplicity of our ProSoft™ soft nasal cannula interface.
Patients can eat, drink, talk, and take oral or aerosolized medications without pausing therapy.

ICU Length of Stay
Vapotherm high velocity therapy could offer you disposition options which could help save ICU beds for patients who truly need them.
In a subgroup analysis, COPD patients on Vapotherm high velocity therapy spent less time in the ICU by comparison to COPD patients on NiPPV. [1]

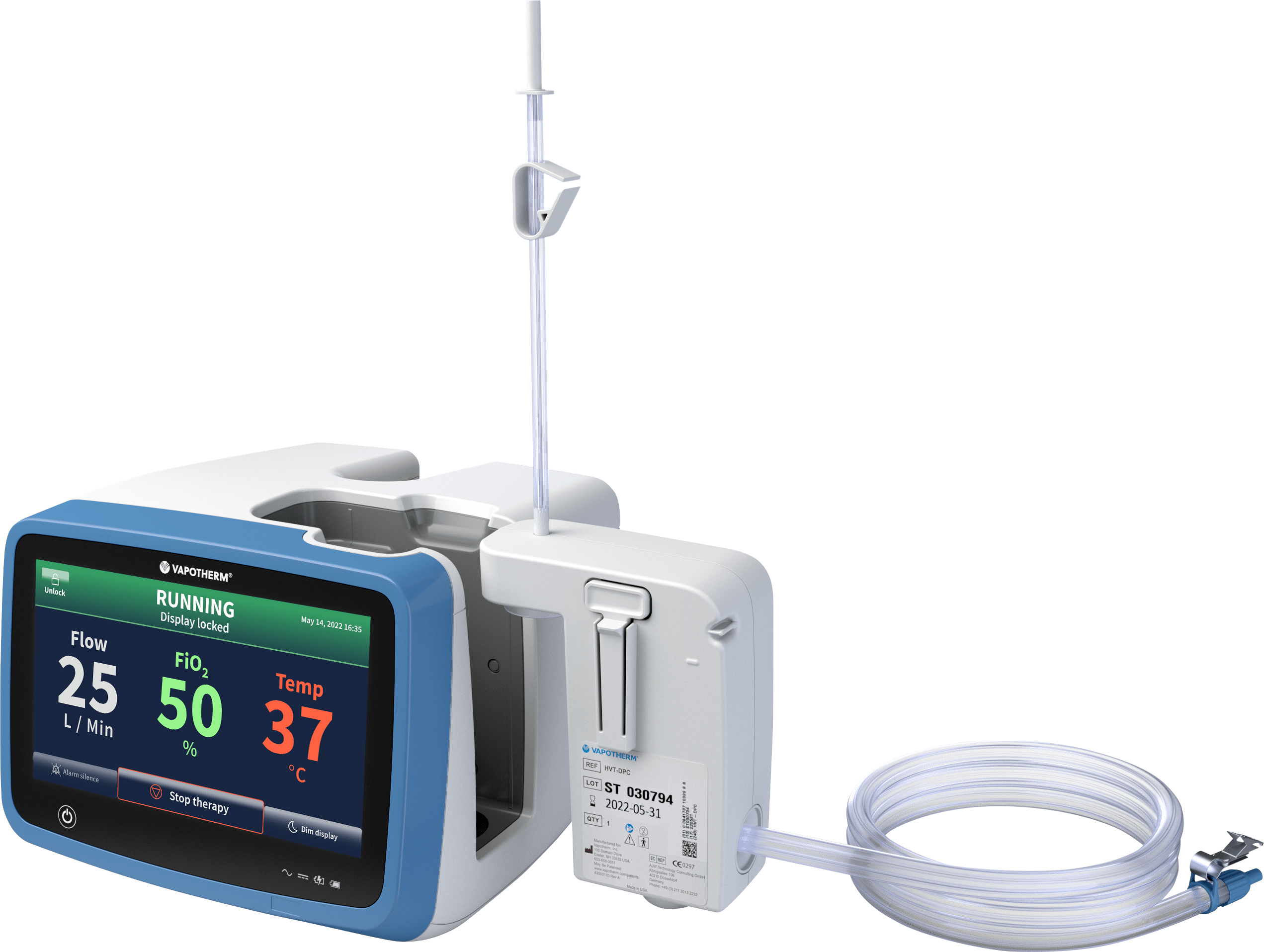
Supporting Ambulation Programs
Get your patients up and moving sooner, rather than later.
There are many clinical and economic benefits to ambulating ICU patients—from potentially improving patient outcomes [2] to reducing length of stay. [7]
The detrimental impacts of bedrest are well-known. [3] [4] [5] [6]
Helping patients ambulate early could help their long-term recovery prospects and also could help your hospital save money. [7] [8]
The Precision Flow® system, equipped with the Vapotherm Transfer Unit, helps provide respiratory support for patients on the move with onboard air and O2 tanks, lithium-ion battery, smart manifold*, and controller.
A feasibility study suggested that these COPD inpatients walked farther, longer, and recovered faster when on Vapotherm high velocity therapy compared to standard oxygen. [9]
Rehabilitation as a Philosophy of Care, Not a Place
Renowned ambulation and rehabilitation educator Nan Nathenson shares her philosophy in the Importance of Early Ambulation eBook
For Patients
- Comfortable and well tolerated
- Patients do not require training for compliance
- Ability to eat, drink, speak, and take oral medication without interrupting therapy
For Providers
- Simple and fast set up
- Easy interface fitting
- Integrated patient safety alarms
For Institutions
- Allows options for patient disposition
- Does not increase risk of intubation
- Reduced intensity of care
Request a Demo
Our team is standing by to teach, guide, and help integrate Mask-Free high velocity therapy into your adult critical care routine.
CAUTION: US Federal law restricts this device to sale by or on the order of a physician. Indications, contraindications, warnings, and instructions for use can be found in the product labelling supplied with each device or at https://vapotherm.com/resources/support/precision-flow-reference/. For spontaneously breathing patients. High Velocity Therapy (HVT) does not provide total ventilatory requirements of the patient. It is not a ventilator. Decisions surrounding patient care depend on the physician’s professional judgment in consideration of all available information for the individual case, including escalation of care depending on patient condition.
SOURCES: [1] Doshi P, Whittle JS, Dungan G et al, The ventilatory effect of high velocity nasal insufflation compared to noninvasive positive-pressure ventilation in the treatment of hypercapneic respiratory failure: A subgroup analysis Lung. 2020 Apr 6. https://doi.org/10.1016/j.hrtlng.2020.03.008 [2] Schweickert, W. D., Pohlman, M. C., Pohlman, A. S., Nigos, C., Pawlik, A. J., Esbrook, C. L., … & Schmidt, G. A. (2009). Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomized controlled trial. Lancet373(9678), 1874-1882. [3] Morris, P. E., Goad, A., Thompson, C., Taylor, K., Harry, B., Passmore, L., & Penley, L. (2008). Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Critical Care Medicine, 36(8), 2238-2243. [4] Van den Berghe, G. (2002). Nueroendocrine pathobiology of chronic critical illness. Critical Care Clinics, 18(3), 509–528. [5] Vanhorebeek, I., & Van den Berghe, G. (2006). The neuroendocrine response to critical illness is a dynamic process. Critical Care Clinics, 22(1), 1–15. [6] Babb, T., Levine, B., & Philley, J. (2012). ICU-acquired weakness: an extension of the effects of bed rest. American Journal of Respiratory and Critical Care Medicine, 185(2), 230-231. [7] Engel HJ, Needham DM, Morris PE, Gropper MA. ICU early mobilization: from recommendation to implementation at three medical centers. Crit Care Med. 2013 Sep;41(9 Suppl 1):S69-80. doi: 10.1097/CCM.0b013e3182a240d5. [8] K Bognar, JW Chou, D McCoy, AL Sexton Ward, J Hester, P Guin, and AB Jena. Financial implications of a hospital early mobility program. Intensive Care Med Exp. 2015 Dec; 3(Suppl 1): A758. Published online 2015 Oct 1. doi: 10.1186/2197-425X-3-S1-A758. [9] Siler, Thomas et al. Assessing the Clinical Effect of High Velocity Nasal Insufflation on Improving Ambulation in Patients with Dyspnea: A Feasibility Study. J Clin Respir Dis Care 2019, 5:2. [10] Black J, Kalowes P. Medical Device-Related Pressure Ulcers. Chronic Wound Care Management and Research Volume 3; 29 August 2016 Volume 2016:3 Pages 91—99. [11] Imbulana DI, Manley BJ, Dawson JA, Davis PG, Owen LS. Nasal injury in preterm infants receiving non-invasive respiratory support: a systematic review. Arch Dis Child Fetal Neonatal Ed. 2018 Jan;103(1):F29-F35. doi: 10.1136/archdischild-2017-313418. Epub 2017 Sep 28. [*] Vapotherm Transfer Unit ‘smart manifold’ not available in all countries where Vapotherm Transfer Unit is available.
