Noninvasive Respiratory Support Selection: Impact on Hospital Reimbursement and Respiratory Department Productivity and Billing

Although thousands of US Short-Term Acute Care (STAC) hospitals commonly use High Flow Nasal Cannula (HFNC) in one or more care areas within their facilities, there remains hospitals that do not use HFNC at all or use it in a limited fashion. This often is due to perceived concerns that greater adoption of the technology in the hospital may negatively impact hospital revenue and respiratory department performance measurements associated with productivity and billing. These concerns are based primarily in HFNC reducing the use of pressure-based therapy alternatives such as NIPPV and CPAP, which are perceived to have preferential hospital reimbursement levels and respiratory department productivity and billing assignments to HFNC.
This article will attempt to answer these concerns using research conducted by an expert, third-party reimbursement consultant and a survey of Respiratory Therapy leaders on their current department practices on productivity and billing, specific to NIPPV/CPAP and HFNC. It does not pretend to be a definitive statement or instructions for HFNC use in a hospital, but rather an aid to help make a more informed decision.
Reimbursement
How is STAC hospital reimbursement/revenue impacted by choosing NIPPV/CPAP or HFNC for respiratory support?
The short answer is that STAC hospital reimbursement in both the inpatient and outpatient settings is not impacted by the respiratory support chosen.
Medicare, the largest US insurer, and most private insurers, have two STAC reimbursement models; one model for inpatient hospital stays and another model for outpatient hospital visits.
Inpatient – Reimbursed based on assignment of an episode of care to a Diagnosis Related Group (DRG) or other similar rate category that defines a specified amount of reimbursement for that DRG or case rate which is not tied to the hospital services provided, including the respiratory support technology used.
Outpatient – Reimbursed based on Common Procedural Terminology (CPT) which is assigned to an Ambulatory Payment Classification (APC) for which the hospital receives a set amount. Although it is true that CPAP has a designated CPT assignment and associated payment (94660, $186.38), in most instances it is not used as the hospital chooses the Critical Care Evaluation & Management (E&M) CPT code at the higher reimbursement rate. In these cases, the CPAP CPT is bundled in the Critical Care Evaluation & Management APC (APC 5041, $734) and the CPAP CPT is not reimbursed.
Medicare reimburses the approximately 1,300 Critical Access Hospitals differently than other STAC hospitals. Medicare, which comprises approximately 75% of all Critical Access inpatient payments, reimburses 101% of Critical Access Hospital costs for inpatient and outpatient stays. Therefore, the respiratory support modality chosen will neither positively or negatively impact hospital reimbursement.
For more information on STAC Hospital reimbursement related to non-invasive respiratory support, please refer to the two white papers recently published on the subject:
- Reimbursement for Non-Invasive Respiratory Support in Hospital Inpatient, Emergency Department and Other Outpatient Settings
- Reimbursement for Non-Invasive Respiratory Support in Critical Access Hospitals
Respiratory Department Productivity and Billing
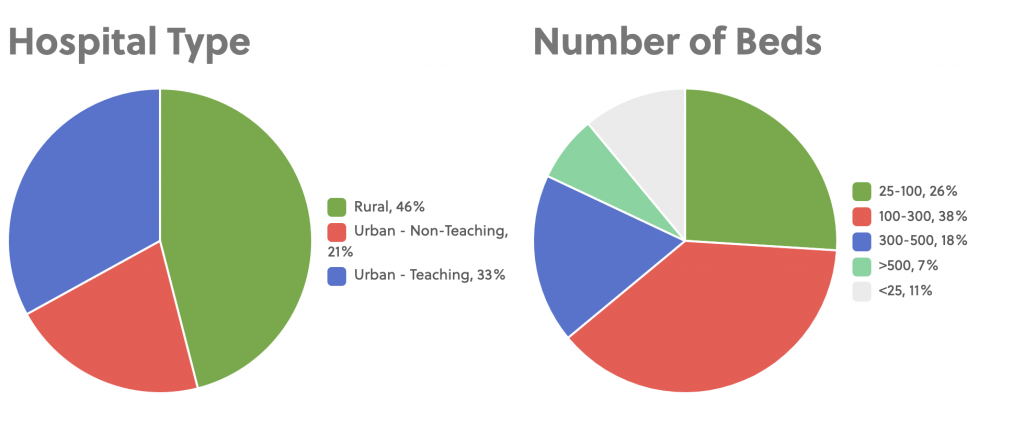
The remaining part of this blog is based on a Respiratory Department Productivity and Billing Survey Vapotherm conducted in May of 2018. 70 Respiratory Department Leaders (i.e. Respiratory Department Directors/Managers/Supervisors, etc.) participated in the survey and they represented a variety of STAC hospital settings and sizes.
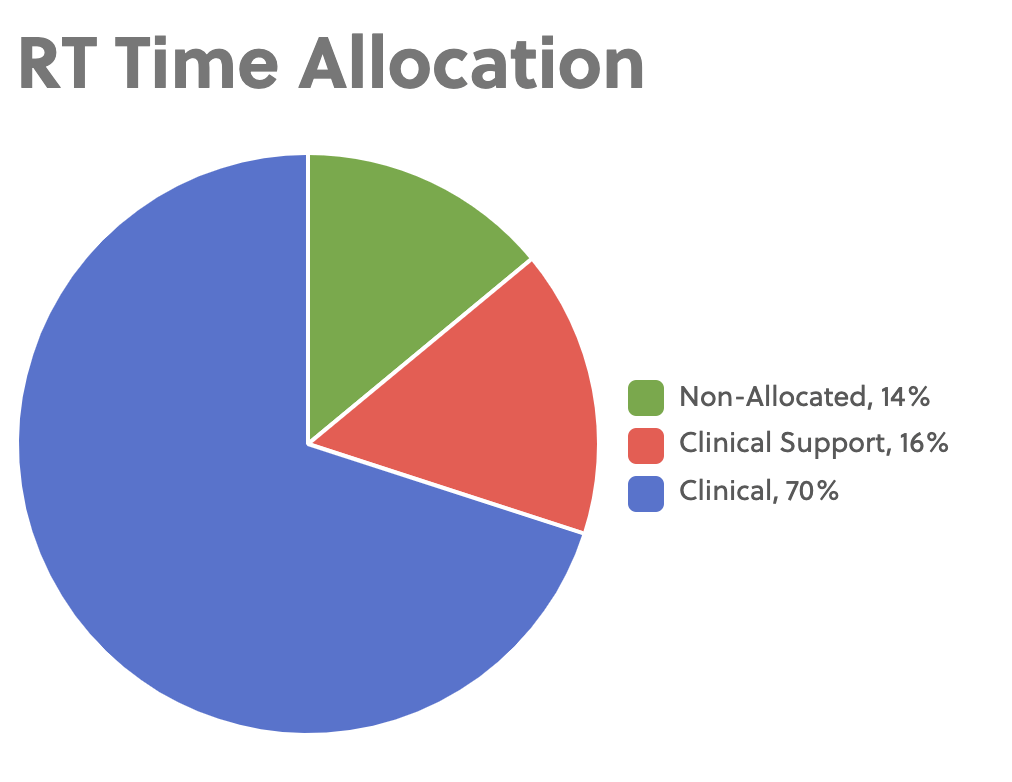
To begin, only about 70% of Respiratory Therapists’ (RT) time is dedicated to clinical activities, with the other 30% spent on clinical support activities (i.e. equipment cleaning and storage, staff development, training, billing, etc.) and non-allocated activities (i.e. travel, communication with HCPs, patients, restroom breaks, etc.).
The majority of RTs workload is in the following clinical activities in order of most amount of time to least amount of time dedicated.
Rank Order of Clinical Activities that comprise RT workload from most to least
1. Invasive Mechanical Ventilation
2. Patient Assessment
3. Medication Delivery
4. Non-invasive Ventilation (CPAP or Bi-level)
5. Aerosol Therapy
6. Heated High Flow Nasal Cannula
7. Bronchial Hygiene
8. Patient Monitoring
9. Airway Care
10. Suctioning
Specific to NIPPV/CPAP and HFNC, RTs currently dedicate approximately twice as much time to clinical activities associated with NIPPV/CPAP (20%) as they do with clinical activities associated with HFNC (10%). According to the survey, when both activities are listed on the Chargemaster, which is a list detailing the official rate charged by a hospital for individual procedures, services and goods, NIPPV/CPAP almost always carries a higher rate to HFNC, averaging approximately five times as high of a charge.
The Chargemaster rates typically are not representative of what a hospital actually gets paid, except in some cases for the uninsured, but may influence RT Department operations if the hospital uses these billing numbers as a key performance metric. According to the survey, approximately 2/3 of Respiratory Departments have the ability to add charges to the Chargemaster working with hospital administration but it is unclear how these rates are determined.
How is Respiratory Department productivity impacted by choosing NIPPV/CPAP or HFNC for respiratory support?
The answer is it is dependent on the STAC Hospital and the system they use to measure productivity, which influences the impact respiratory support choice has on Respiratory Department productivity measures.
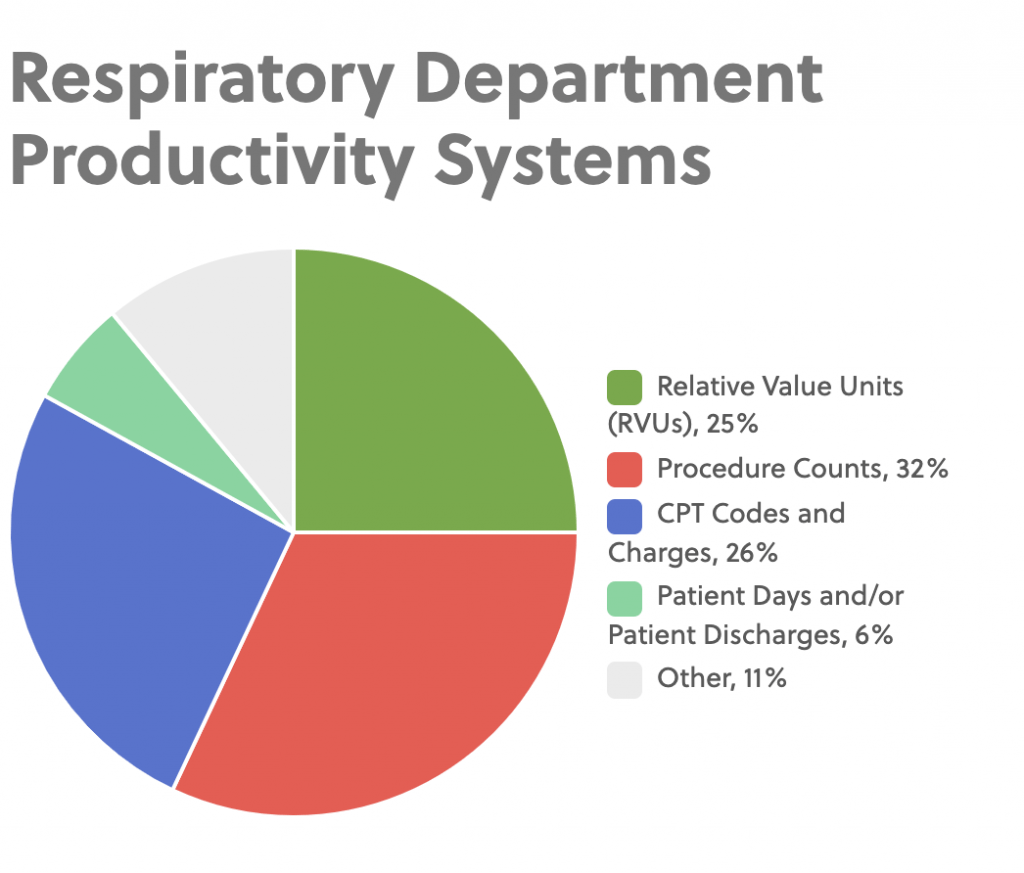
Procedure Counts (32%) – Assigns points to clinical activities. Typically, one point equals a certain minute value (Between 10-15 minutes). Approximately 2/3 of respondents in the survey that use procedure counts give a weighted point total based on the type of clinical activity performed while the other 1/3 assign one point to a clinical activity regardless of the type. HFNC is a valid procedure at 57% of facilities in the survey that use the procedure count system.
CPT Codes and Charges (26%) – Use billable procedures based on CPT codes. Approximately 2/3 of the respondents that use this system are unable to get credit for any clinical activity that does not have a CPT assigned. The remaining 1/3 use either the miscellaneous code 94799 for clinical activities that do not have a specific CPT code or have a separate system to get productivity credit for these clinical items. About 1/3 of respondents either do not account for or do not use HFNC at their facilities, while 2/3s say they use an oxygen CPT code, have created a HFNC CPT code, use the miscellaneous CPT code or have another way for getting productivity credit for the use of the technology.
Relative Value Units (RVUs) (25%) – Assign times to each activity that is typically based on the American Association of Respiratory Care (AARC) Uniform Reporting Manual (33%), hospital specific time-motion studies (20%) or a combination of the two (40%). The median minute totals for different clinical activities associated with NIPPV/CPAP and HFNC from respondents who use the RVU system follow. (Note: Small n=12)
| Clinical Activity | NIPPV/CPAP | HFNC |
|---|---|---|
| Set-up/Initiation | 17.5 | 10 |
| Patient/System Assessment | 10 | 5 |
| Setting or Device Adjustment | 1 | 0.5 |
These productivity scores may be indicative of historical views on the role of these two therapies and may not reflect recent clinical evidence to suggest HFNC as a viable alternative to NIPPV/CPAP to treat the same type and acuity of patients.
Patient Days or Discharges (6%) – Broad metrics often to benchmark hospitals but infrequently used to measure Respiratory Department productivity. All four survey respondents that use this system to determine department productivity used different measures; from number of RT hours per patient day to X number of RTs per patients to X number of RTs per procedure.
Other (11%) – Two respondents did not currently use productivity measures at their facilities and the other four should have classified themselves either under the CPT Codes and Charges (2) or RVUs (2) based on their response to how productivity is calculated at their facility.
Therefore, to understand whether an RT Department productivity is impacted by their choice of NIPPV/CPAP or HFNC, it is important first to determine what type of productivity system the hospital uses as different systems give the Respiratory Department more or less say of what productivity is assigned to a clinical activity. Hospitals that use CPT Codes and charges for productivity seem to be the most restrictive and favor NIPPV/CPAP while hospitals that use procedure code systems or RVU systems appear to give RT Leaders greater ability to adjust productivity assignments based on the realities of their departments.
With the exception of hospitals that use the CPT Code and Charges system, what role does billing play in a Respiratory Department?
Respiratory Department billing is used for one or more of the following reasons for the hospitals surveyed.
Revenue – Critical Access hospitals need to account for the specific activities performed and the capital and disposable product used to calculate hospitals costs which is the basis of their Medicare reimbursement. Normal STAC hospitals also use billing to generate revenue from patients not covered under the DRG system as well to have an accurate record of activities to support the DRGs assigned.
Staffing – Billing is used as a secondary measure of productivity and appropriate staffing for hospitals that use non-CPT Codes and Charges productivity systems. It is unclear if billing is just another way of representing the productivity system numbers or if it a completely different measure that influences staffing.
Analytics – Hospitals use information to run reports to identify macro and seasonal trending over time in the hospital as well as to benchmark itself against other hospitals in the system or in the larger market.
None – Hospitals that do not use a CPT Codes and Charges for productivity admitted to not use billing for any purpose.
Discussion
It is the responsibility of the Respiratory Department to compare the clinical and economic impacts of bringing a new respiratory modality or technology into their hospital. There has been an increase in high quality clinical evidence over the last few years to support HFNC as a more comfortable, viable alternative to pressure-based therapies to treat respiratory distress in neonates to adults. As Respiratory Departments look to adopt or expand the use of the technology in their hospitals, there are concerns about the impact this will have on hospital department reimbursement and Respiratory Department productivity and billing, specifically as it relates to department performance and staffing.
In regards to hospital reimbursement, there is no penalty to the hospital by choosing HFNC over another therapy modality under the Medicare DRG and APC prospective payment systems and cost-based payment system for STAC hospitals for Critical Access Hospitals respectively. There can be more of an impact to Respiratory Department productivity and billing based on which type of productivity measures the hospital employs, especially if it is based on strict CPT coding, however, in most cases the Respiratory Department can work with hospital administration to set the productivity and internal billing numbers to properly represent the relative time and value of using HFNC. Based on the survey data, hospitals currently give greater productivity scores and billing rates to pressure-based therapies (NIPPV/CPAP) compared to HFNC. Given that HFNC is being used more to treat the same type and acuity of patients, it may be worthwhile for Respiratory Departments to look at these numbers again so as not to incentivize the use of one modality over the other simply due to productivity scores.