High Velocity Therapy in the Emergency Department
One Mask‐Free Respiratory Tool.
Multiple Levels of Patient Acuity

Velocity for a Fast‐Paced ED
With the clinical ease and capabilities of typical high flow plus clinical proof in a wide range of acutely ill patients, Vapotherm high velocity therapy is a trusted tool in emergency rooms around the world for treating patients with type 1 and type 2 respiratory failure.
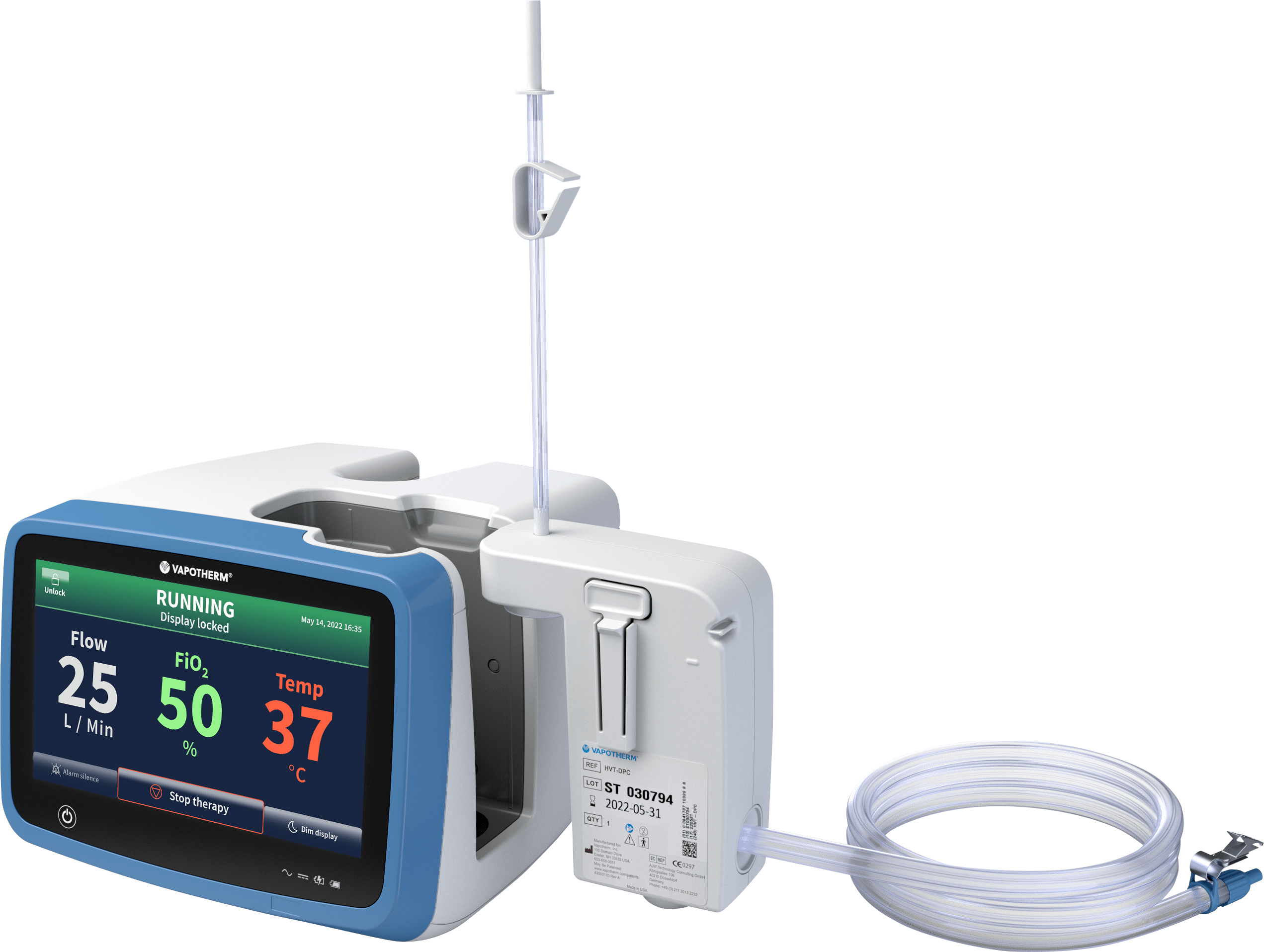
The Precision Flow® system can be patient-ready in minutes, portable with the Vapotherm Transfer Unit, and allows for multiple patient disposition options to support your ED throughput.

One Respiratory Tool,
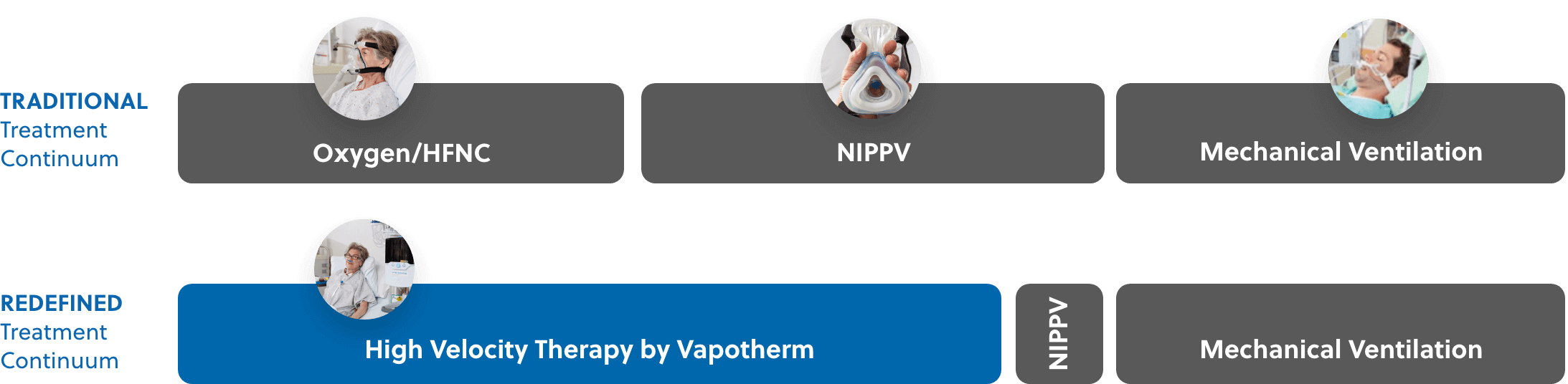
A Redefined Continuum of Care
Vapotherm high velocity therapy, an advanced form of high flow nasal cannula, can be used to provide mask‐free respiratory support.
This one respiratory tool provides respiratory support for patients in a wide array of respiratory distress acuity – including hypercapnia, hypoxemia, or dyspnea. Therapy with the Precision Flow® system can be started quickly with precise control of flow, oxygen, and temperature while maintaining optimal humidity.
Increased Acuity Levels of Respiratory Distress
Disclaimer: High Velocity Therapy is not intended to provide the total ventilatory requirements of the patient. For spontaneously breathing patients only.

Mask-Free Respiratory Support
Not all patients tolerate mask-based therapies well. Mask intolerance causes up to 33% of NiPPV Failures. [1]
Vapotherm high velocity therapy is a comfortable choice for a host of respiratory distress patients for whom a mask may not be ideal. These patients can include pediatric patients, elderly patients, patients with anxiety, claustrophobia, or even facial hair prohibiting proper mask seal.
A Step Up for Using Step Down
Patients on high velocity therapy can safely be managed on the floor or step‐down unit. With more options for disposition, your ED could improve patient flow through your emergency department resulting in faster throughput, shorter wait times, and less stress on you and your department.
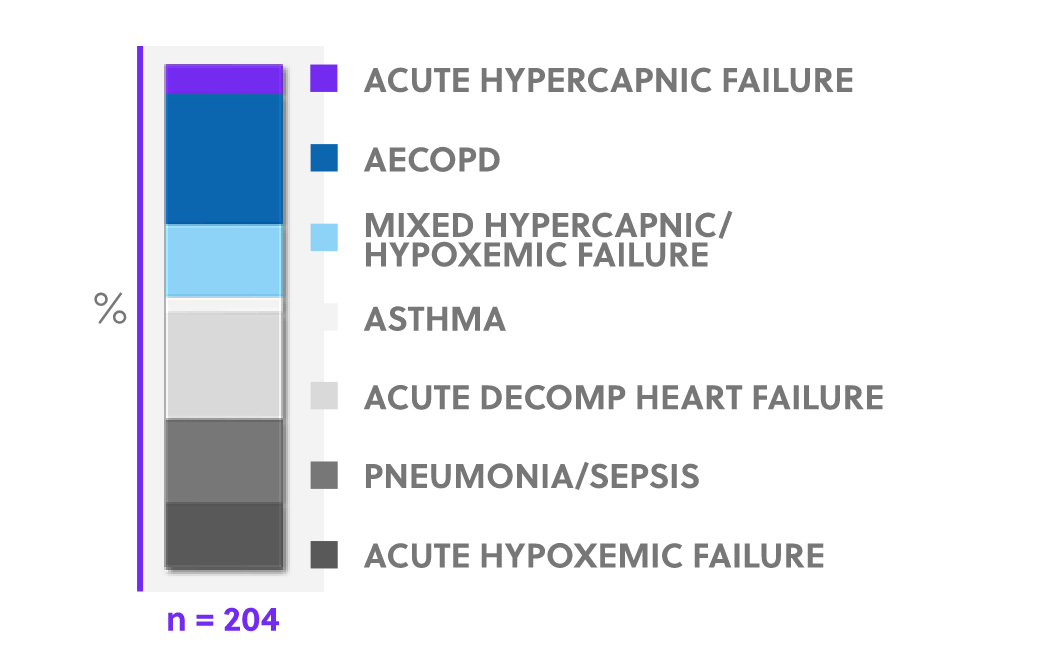
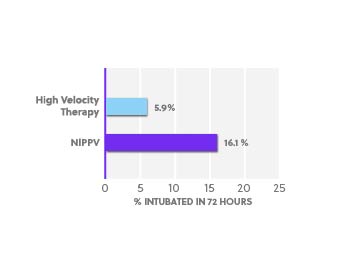
Clinically Proven Alternative to NiPPV for spontaneously breathing patients
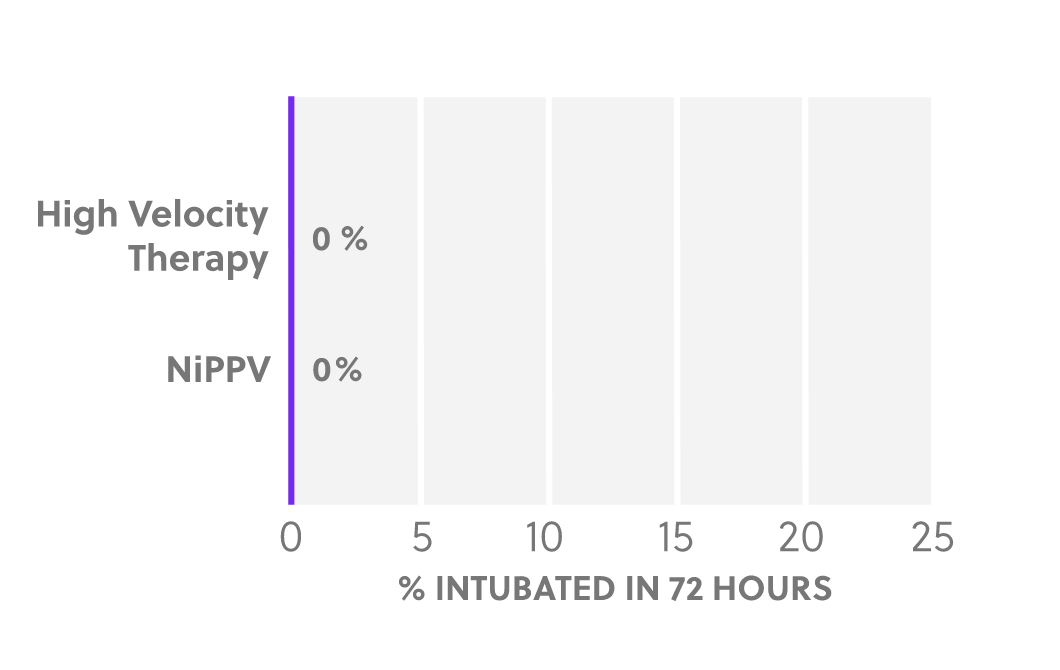
A randomized multi-center controlled trial of adults presenting in the emergency department with undifferentiated respiratory distress showed Vapotherm high velocity therapy – Mask‐Free NIV – to be non-inferior to the gold standard non-invasive positive pressure ventilation (NiPPV). [2] [3]
All Newcomers in Respiratory Distress
Intubation Rates

High velocity therapy does not provide the total ventilatory requirements of the patient. For spontaneously breathing patients only.
Mask-Free Respiratory Support for COPD and CHF Patients
Whether acute hypercapnia from COPD, dyspnea, or respiratory distress associated with COVID-19, Vapotherm high velocity therapy is one user‐friendly tool that helps you effectively and safely support your patients without some of the limitations of the traditional non‐invasive standard of care.
COPD Subgroup Analysis
CHF Subgroup Analysis
 Adapted from Doshi 2020
Adapted from Doshi 2020
High velocity therapy does not provide the total ventilatory requirements of the patient. For spontaneously breathing patients only.
Comfortable for Patients,
User‐Friendly for Clinicians
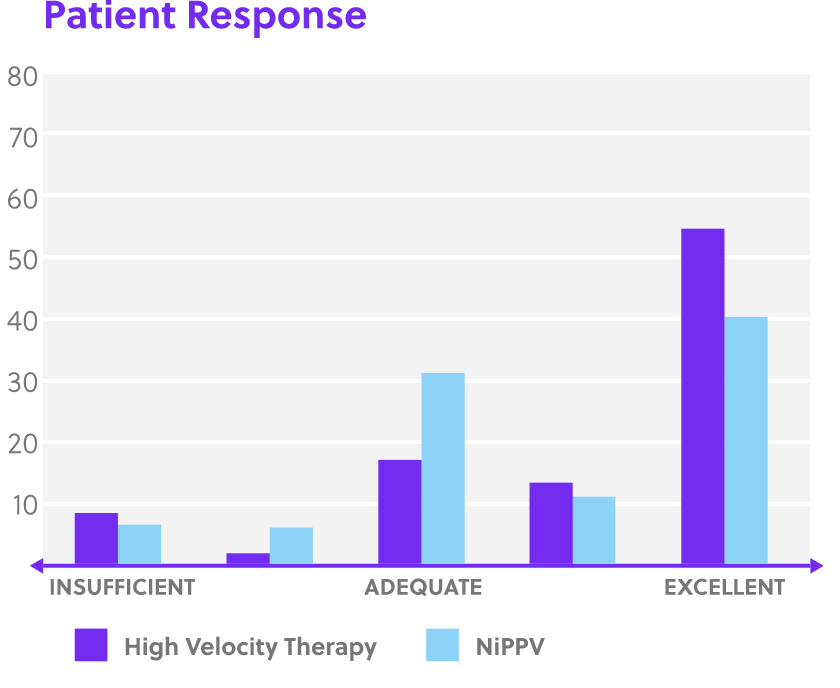
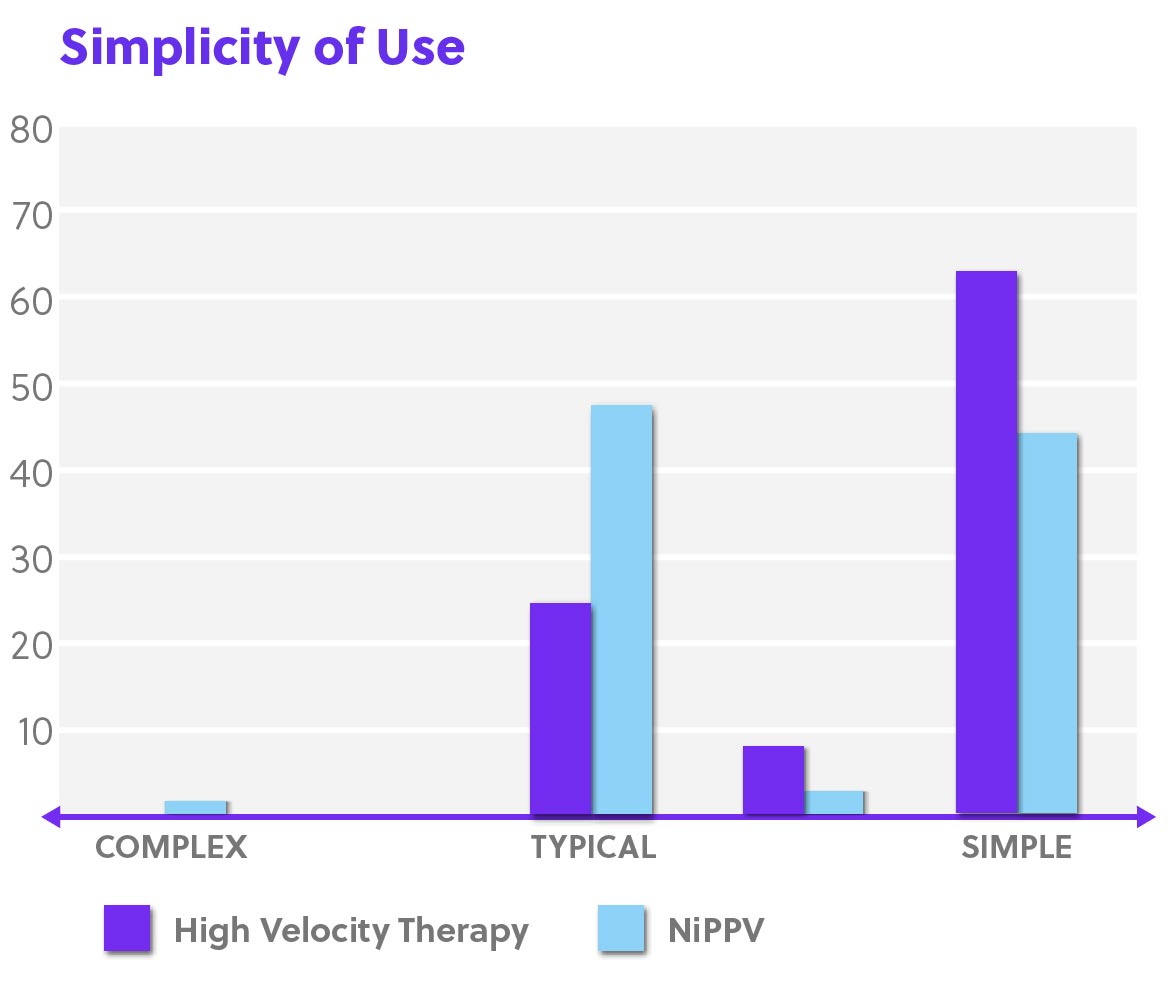
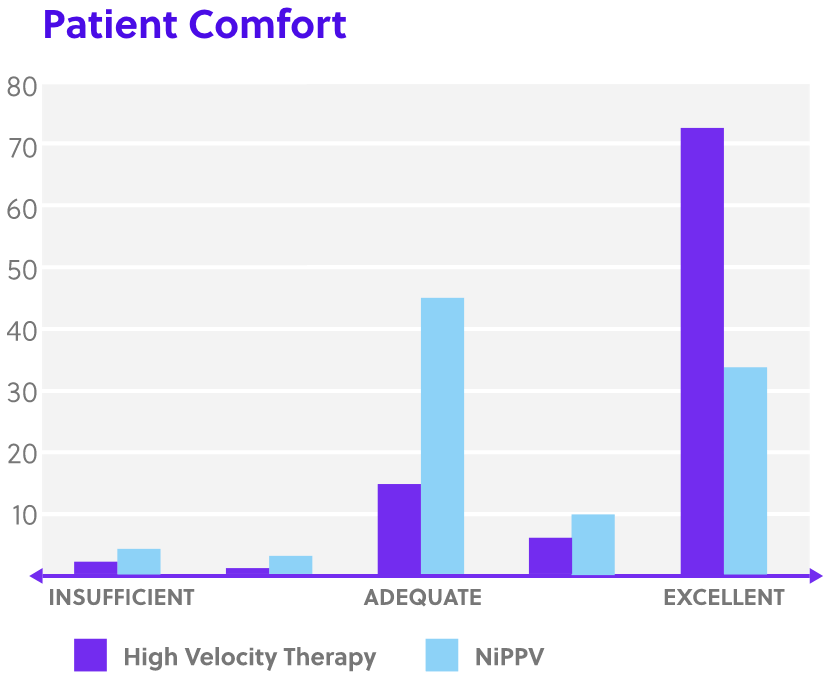
Disclaimer: Perception of patient response, patient comfort and simplicity of use as reported by physicians in Doshi, et al. study. [4]
For Patients
- Comfortable and well tolerated
- Patients do not require training for compliance
- Ability to eat, drink, speak, and take oral medication without interrupting therapy
For Providers
- Simple and fast set up
- Easy interface fitting
- Integrated patient safety alarms
For Institutions
- Allows options for patient disposition
- Does not increase risk of intubation
- Reduced intensity of care

More Freedom to Focus on your Patients
“We initially decided to start using the Vapotherm in our Emergency Department because we were educated on the fact that not all patients who are having a COPD exacerbation necessarily need non-invasive positive pressure ventilation. Now, we use the Vapotherm instead to rescue these patients much more comfortably and less invasively.”
Shirley Gresham, RRT, RCP
Cardiopulmonary Supervisor
Norman Regional Health System

No Mask. No Problem. Mask-Free NIV.
Dr. Aisha Terry presents “No Mask. No Problem. Mask-Free NIV”. In this presentation you’ll get a better understanding of Mask-Free NIV and the mechanisms of action for high velocity therapy.
Respiratory Therapists can earn 1 AARC RT CRCE.
Nurses can earn 1 Contact Hour.
Request a Demo
Our team is standing by to teach, guide, and help integrate Mask‐Free high velocity therapy into your Emergency Department.
CAUTION: US Federal law restricts this device to sale by or on the order of a physician. Indications, contraindications, warnings, and instructions for use can be found in the product labelling supplied with each device or at https://vapotherm.com/resources/support/precision-flow-reference/. For spontaneously breathing patients. High Velocity Therapy (HVT) does not provide total ventilatory requirements of the patient. It is not a ventilator. Decisions surrounding patient care depend on the physician’s professional judgment in consideration of all available information for the individual case, including escalation of care depending on patient condition.
SOURCES: [1] Carron M et al, Complications of non-invasive ventilation techniques: a comprehensive qualitative review of randomized trials, British Journal of Anaesthesia, 110 (6): 896–914 (2013). [2] Doshi P, Whittle JS, Bublewicz M, et al. High-Velocity Nasal Insufflation in the Treatment of Respiratory Failure: A Randomized Clinical Trial. Ann Emerg Med 2018;72:73-83 e5 [3] Doshi P, Whittle JS, Dungan G et al, The ventilatory effect of high velocity nasal insufflation compared to noninvasive positive-pressure ventilation in the treatment of hypercapneic respiratory failure: A subgroup analysisLung. 2020 Apr 6. https://doi.org/10.1016/j.hrtlng.2020.03.008 [4] Haywood, Steven T, Jessica S. Whittle, Leonithas I. Volakis, George Dungan II, Michael Bublewicz, Joseph Kearney, Terrell Ashe, Thomas L. Miller, Pratik Doshi. “HVNI vs NIPPV in the treatment of acute decompensated heart failure: Subgroup analysis of a multi-center trial in the ED.” The American Journal of Emergency Medicine, 2019. https://doi.org/10.1016/j.ajem.2019.03.002