Dr. Jessica Whittle shares her firsthand experience using Vapotherm High Velocity Therapy on a severely hypercapnic patient.
“Everything I thought I knew about ventilating patients was called into question. I had always been taught you use pressure to stent open airways, I still believe sometimes you do. But for a lot of patients there is a better option. It [high velocity therapy] was more comfortable, it was more effective.”
– Jessica Whittle, MD
VP of Clinical at Vapotherm, Chief Medical Officer
Learn more about High Velocity Therapy for Hypercapnic Patients
We recognize that this concept is revolutionary, so we’ve compiled resources to help you champion effective and comfortable care in your department.
Hypercapnia Clinical Research
2018 – Doshi et al. shows high velocity therapy similarly effective to NiPPV for undifferentiated respiratory failure in adults.
2020 – Doshi et al. subgroup analysis suggests high velocity therapy may be similarly effective to NiPPV for adult COPD patients
2021 – Plotnikow et al. supports high velocity therapy as a first-line support on severely hypercapnic COPD patients and independently validates Doshi findings
2023 – Kacinski et al. quantifies and measures CO2 removal using a 3D airway model, demonstrating that reducing CO2 levels in the upper airway is dependent upon cannula design
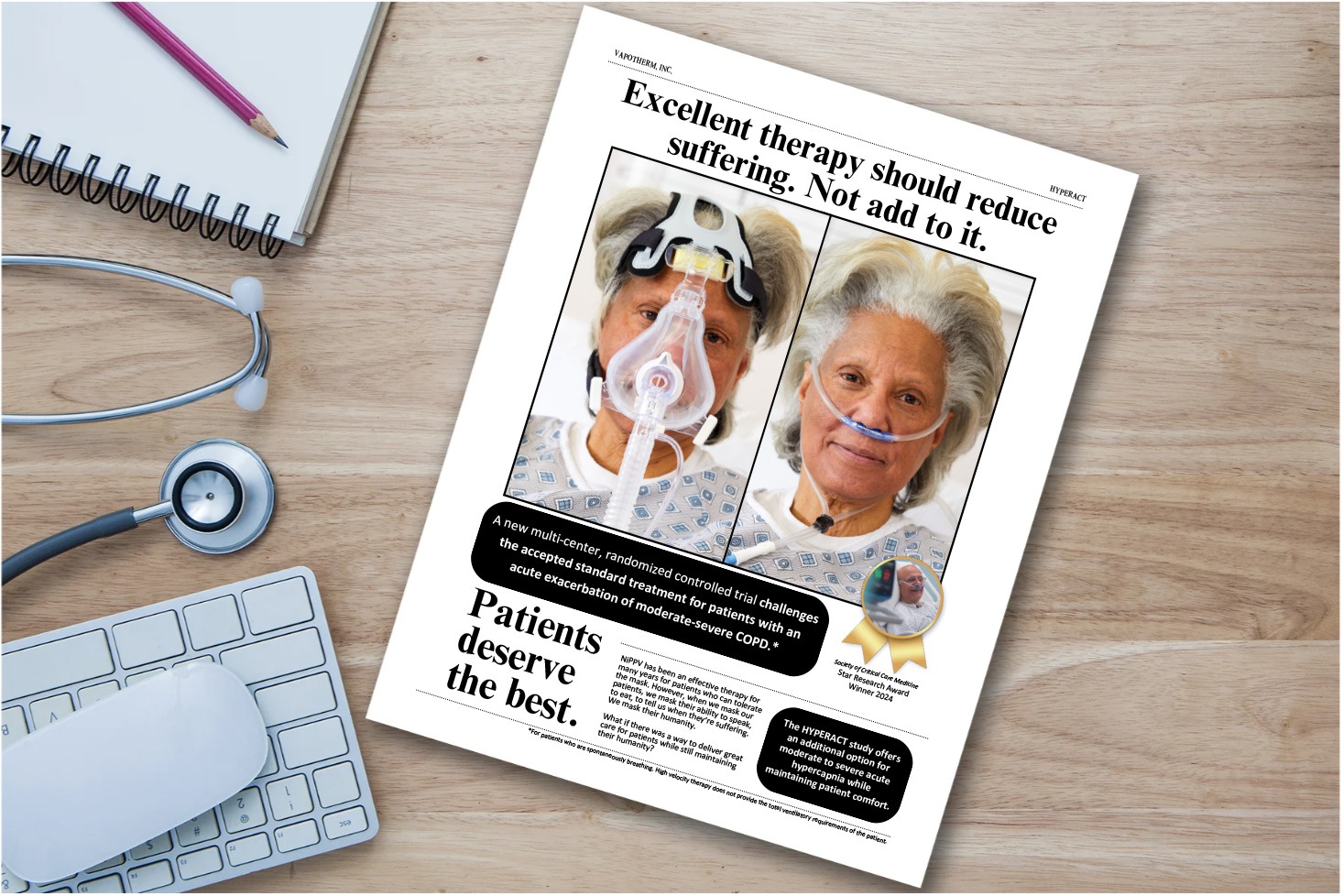
2024 – HYPERACT – We know that high velocity therapy is effective for COPD exacerbations, but how severe of an exacerbation?
This multicenter, randomized controlled trial compared NiPPV to high velocity therapy for moderate to severe COPD patients. Patients in this study had a pCO2 of 60 mmHg or higher, venous pH of 7.0-7.35 and presented with acute hypercapnic respiratory failure.
The study hasn’t been published yet – would you like to be updated on the findings? Join our email list here.
Download your free HYPERACT Document
We’ve created a document to help Respiratory Therapists advocate to physicians the use of high velocity therapy for hypercapnic patients.
The next time a patient is struggling to tolerate a mask-based therapy, we hope you find this tool helpful when you ask your teammates, “Hey, why don’t we try high velocity therapy?”
Your teammates may ask you….
- What clinical evidence supports hypercapnic use?
- Moderate to severe COPD patients?
- How does high velocity therapy support ventilation?
All that and more in this free downloadable so you can advocate for your patients!
This may be a novel concept to some – you’re not alone.
Connect with a team member if you have questions on what makes high velocity therapy different and possible cost savings of high velocity therapy compared to mask-based therapies.
Vapotherm Academy Hypercapnia Courses
You and your colleagues can keep learning with Vapotherm Academy’s FREE CEU courses.
1 CRCE/1 Nurse CE
1 CRCE/1 Nurse CE
1 CRCE/1 Nurse CE

This eBook includes articles on:
“What is High Velocity Therapy?” by John Walsh, CRT
“COPD Patients and Wound Care Implications with High Velocity Therapy” by Jeanne Pettinichi, MSN, RN, CPN, CPEN
“Treating COPD Patients with High Velocity Therapy” by Kirk Hinkley, MD, FACEP
“Ventilatory Support via an Open System – How Does it Work?” by Amrit Kahlon, MD
Hypercapnia Blog Articles
- Presenting HYPERACT
 We invite you to learn about this recent multi-center, randomized controlled trial (RCT) which challenges the accepted standard treatment for patients with an acute exacerbation of moderate-severe COPD.
We invite you to learn about this recent multi-center, randomized controlled trial (RCT) which challenges the accepted standard treatment for patients with an acute exacerbation of moderate-severe COPD. - New Study Adds Evidence for Use of Vapotherm® High Velocity Therapy as First-Line Support on Severely Hypercapnic COPD Patients
 Plotnikow concludes that high velocity therapy is an effective tool for reducing RR in COPD patients with acute hypercapnic respiratory failure.
Plotnikow concludes that high velocity therapy is an effective tool for reducing RR in COPD patients with acute hypercapnic respiratory failure. - Rethinking Ventilation — Do you always need pressure?
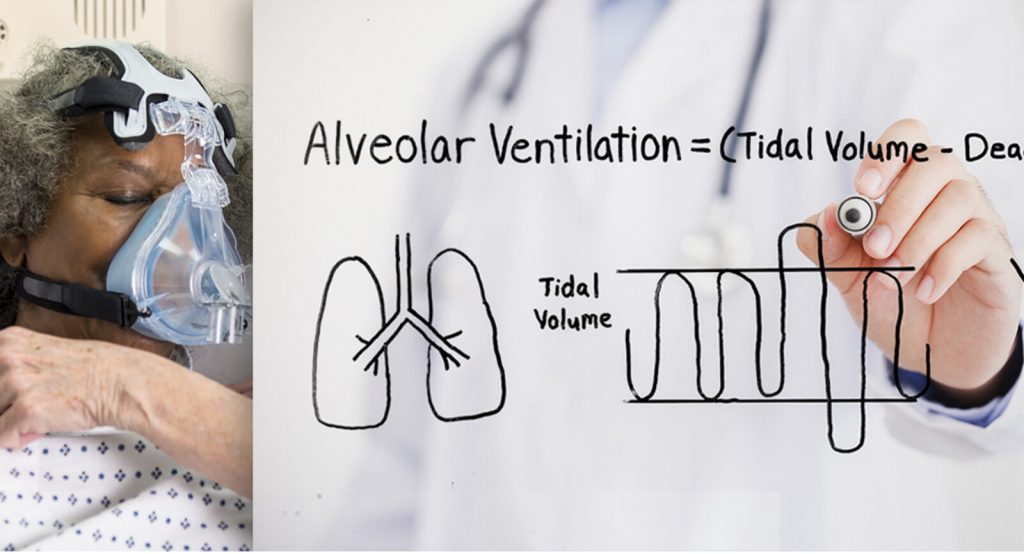 The simple answer to the question of whether you can achieve alveolar ventilation with minimal pressure is yes – high velocity therapy.
The simple answer to the question of whether you can achieve alveolar ventilation with minimal pressure is yes – high velocity therapy. - 40 vs 60 L/min: What’s the Difference Between Vapotherm® High Velocity Therapy and High Flow Nasal Cannula?
 By quickly clearing the upper airway dead space of end-expiratory gas rich in CO2, high velocity therapy helps patients breathe directly from a fresh gas reservoir and thereby reduces their WOB.
By quickly clearing the upper airway dead space of end-expiratory gas rich in CO2, high velocity therapy helps patients breathe directly from a fresh gas reservoir and thereby reduces their WOB.

Our team is standing by to teach, guide, and help you get the most out of the HVT 2.0 system.
Request a Demo
CAUTION: US Federal law restricts this device to sale by or on the order of a physician. Indications, contraindications, warnings, and instructions for use can be found in the product labelling supplied with each device or at https://vapotherm.com/resources/support/precision-flow-reference/. For spontaneously breathing patients. High Velocity Therapy (HVT) does not provide total ventilatory requirements of the patient. It is not a ventilator. Decisions surrounding patient care depend on the physician’s professional judgment in consideration of all available information for the individual case, including escalation of care depending on patient condition.
Study Limitations:
Neither the participants, providers, nor assessors were blinded to the treatment arms, but all were blinded prior to allocation and enrollment
Patients with respiratory distress due to mixed reasons may have been included, however, undifferentiated complaints are typical in ED setting
Patients were able to provide verbal assent and not in imminent respiratory arrest. Caution should be exercised when extrapolating the results of this study to patients in extreme distress
All patients received standard care, however variability exists among clinicians regarding what constitutes standard of care
Study utilized a subjective measure – degree of dyspnea – as primary outcome. However it was augmented by quantitative pH and PCO2 values
Study conducted during COVID-19 pandemic, acute phase