What are Ventilator-Associated Pneumonias/Ventilator-Associated Events and How to Reduce Their Prevalence in Your Hospital
It is difficult to pin down the exact prevalence of Ventilator-Associated Pneumonia (VAP)/Ventilator-Associated Events (VAE), but it is widely agreed that they are among the most common nosocomial events in the ICU, leading to decreased patient outcomes and increased length of stay.[1,2,3] Hospitals are eager to reduce the incidence of these events, but to accomplish this, it is important to first understand how they are defined, diagnosed, what impact they have on the patient and hospital, and what possible precautions can be taken.
What is Ventilator-Associated Pneumonia and What is a Ventilator-Associated Event?
According to the Clinical Practice Guidelines on the Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia, published in 2016 by the Infectious Diseases Society of America and the American Thoracic Society, VAP is “a pneumonia occurring >48 hours after endotracheal intubation.”[1] However, the guidelines acknowledge that there is no single standard in defining VAP. The range of definitions and diagnostic criteria used in reporting VAP has led to difficulty studying the subject, as well as to a degree of controversy.[2,4] The definition used impacted the prevalence of diagnosis and also led to VAP occasionally being lumped in with other disease categories, making tracking even more difficult. For example, Hospital-Acquired Pneumonia (HAP) has often been regarded as an umbrella term that encompasses VAP and therefore much literature on the topic refer to them as overlapping kinds of infections. But the updated 2016 management guidelines define HAP and VAP as separate categories with the former exclusively encompassing pneumonias not associated with mechanical ventilation.[1]
Due in part to the inconsistencies resulting from the variety of definitions of VAP, the National Healthcare Safety Network (NHSN) — which is part of the Centers for Disease Control and Prevention (CDC) and is tasked with collecting data on healthcare-associated infections (HAI) — implemented a new definition algorithm in 2013 for surveillance of VAP in the adult population.[5] This algorithm introduced the term of Ventilator-Associated Event (VAE) into the literature.
According to the CDC, a VAE is classified as a “deterioration in respiratory status after a period of stability or improvement on the ventilator, evidence of infection or inflammation, and laboratory evidence of respiratory infection.” These parameters permit for a more objective definition used in reporting and surveillance of VAP, but the CDC stresses that this is not a clinical algorithm and is “not intended for use in the clinical management of patients.”[6] In other words, VAEs did not supplant the existence of VAPs and while all VAPs are VAEs, not all VAEs are necessarily VAPs.
How is Ventilator-Associated Pneumonia Diagnosed?
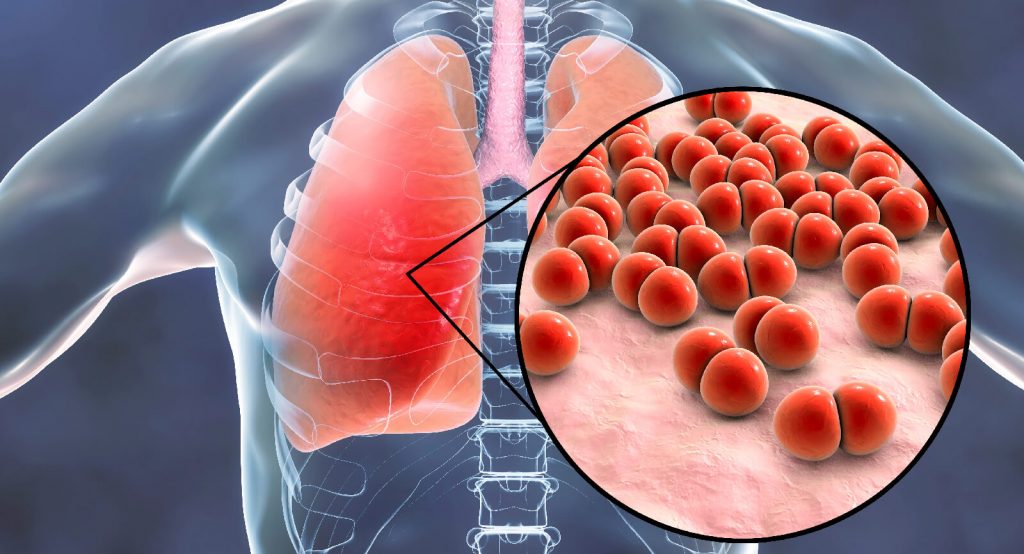
Given the complicated landscape of VAP definitions, it is no surprise that there is no universally accepted criteria for VAP diagnosis. VAP can occur when the lower airway’s natural protective mechanisms have been compromised by an endotracheal tube or tracheostomy in the course of intubation for the purpose of mechanical ventilation.[9] It is generally agreed that a combination of clinical, radiological, and microbiologic diagnostic approaches can be employed, with the first two being mandatory and the lab data being optional.[3]
A 2008 qualitative literature review conducted by Rea-Neto and colleagues found that microbiologic data did not improve accuracy of diagnosis.[9] The 2016 clinical guidelines on the management of adults with hospital-acquired and ventilator-associated pneumonia largely still support this finding. In their recommendations for microbiologic diagnosis, the authors state that evidence for invasive and non-invasive microbiologic sampling in suspected VAP patients is low quality while evidence for treating patients based on clinical and empirical diagnoses is moderate-quality.[1]
The CDC’s surveillance algorithm for detecting VAEs takes into consideration a patient’s daily minimum positive end-expiratory pressure (PEEP), daily Fi02, and the number of vent days.[6] As with the change of definition, these criteria are more objective, but again the CDC emphasizes the algorithm is meant for surveillance only and not as a clinical recommendation.
Is VAP a “Never Event”?
Despite the controversy and subjectivity inherent in VAP diagnoses, there is overall consensus that VAP is a serious event that hospitals should strive to minimize or eliminate. This is why there has been an ongoing discussion on whether VAP should be considered a “never event.”[12]
The Centers for Medicare and Medicaid Services (CMS) defines “never events” as “serious and costly errors in the provision of health care services that should never happen,” listing as examples surgery on the wrong body part—preventable mistakes that lead to serious harm to the patient and increased medical costs.[10] Starting in 2008, CMS has made policy changes which dictate that hospitals will no longer receive reimbursement for certain “never events.” Even though it has been under consideration since the inception of the list, VAP is not on the current list of CMS’s “never events.”[11,12]
Nevertheless, VAP is a serious event that further compromises the health of already critically ill ICU patients. Due to the problems in studying VAP outlined above, it is not possible to state with certainty what the increased mortality rate is in patients who develop VAP. An extensive 2006 literature overview titled “Ventilator-Associated Pneumonia: Diagnosis, Treatment, and Prevention” by Steven M. Koenig and Jonathon D. Truwit found that reported attributable VAP mortality rates range anywhere from 0%-50.[3] More recent estimates have decreased these numbers to 9%-13%.[7] The underlying disease states prior to intubation play a role in the attributable risk of death.
Cost to Hospital
Even though the mortality rates of VAP are not as high as once thought, the fact that VAP incidences lead to increased length of stay and increased treatment cost is not disputed.[1,3,13]
Estimates yet again vary depending on definitions and variables studied. Koenig and Truwit’s overview estimates an increased cost of $5,000 – $20,000 per VAP diagnosis.[3] However, more recent studies have placed the number higher, especially since the cost of hospitalization has increased in the last ten years.
In a retrospective matched cohort analysis of VAP patients vs controls without VAP, published in 2010, Marcos I. Restrepo and colleagues found that median losses to hospitals were $32,140 for case patients and $19,360 for control patients (P=.151). The median ICU length of stay was 18.5 days in case patients vs 8.0 days (P <.001) and the median duration of hospitalization was 26.5 days vs 14.0 days (P<.001) respectively.[13]
This study, titled “Economic Burden of Ventilator-Associated Pneumonia Based on Total Resource Utilization,” looked not only at length of stay, but at overall services required in VAP cases. Table 1 depicts the services with the highest median cost — the calculations are based on the study results.
Table 1: Increase of Median Cost for VAP Patients Per Resource
Reduction Through Prevention
With adverse patient outcomes and increased costs attributable to VAP, hospitals have been trying to reduce prevalence through VAP Bundles. The measures suggested in these bundles contain, but are not limited to the following:
- Alcohol-based hand washing policy
- Early discontinuation of invasive devices
- Reduce reintubation rates
- Use of oropharyngeal vs. nasopharyngeal feeding tubes
- Semi-recumbent patient positioning (30-45°)
- Endotracheal tube cuff pressure ~ 20 cm H2O
- Early tracheostomy
- Small bowel feeding instead of gastric feeding
- Prophylactic probiotics[7]
All of the above have been shown to be, to some degree, effective in reducing VAP prevalence, though the evidence for each varies.
The evidence on the effectiveness of VAP bundles themselves varies. For example, a retrospective, population-based cohort study published in 2013 by Ding and colleagues concluded that implementation of bundles had no effect on VAP prevalence.[4]
On the other hand, a study titled “Sustained Reduction of Ventilator-Associated Pneumonia Rates Using Real-Time Course Correction With a Ventilator Bundle Compliance Dashboard” and published in 2015 by Thomas R. Talbot and colleagues found greater success. The study design included a computerized dashboard that allowed clinicians to easily see (via color coding) which bundle components were completed and which ones were pending — a set up that encouraged real-time adherence. The study encompassed a total of 87,537 and the authors conclude that the prevention program was “associated with significant sustained decreases in VAP rates and an increase in bundle compliance among adult ICU patients.”[14]
The success of any VAP bundle is contingent on implementation and continued adherence. The results of a cross-sectional survey found that reduction of VAP was associated with the number of bundle elements that were adhered to, while the presence of a full-time epidemiologist had significant associations with decreased VAP incidences.[15]
Like there is no gold standard for VAP diagnoses, there also is no silver bullet for its prevention. But it is important to note that there are sometimes options available prior to the use of mechanical ventilation. For example, Koenig and Truwit, in their overview note that use of non-invasive ventilation (NIV) is associated with decreased incidence of nosocomial pneumonia in general. Although they do write that “clinicians have significant reluctance to initiate NIV, perhaps because of patient intolerance or increased resource consumption (nursing and respiratory therapy)” it should go without saying that the best prevention of VAP is avoiding intubation whenever possible.[3]
Learn more about the mask-free alternative to NiPPV
REFERENCES
[1] Kalil, AndreC. et al. “Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society.” Clinical Infectious Diseases. 2016 Sept; 63(5): e61-e111. https://academic.oup.com/cid/article/63/5/e61/2237650
[2] Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. American Journal of Respiratory and Critical Care Medicine. https://www.atsjournals.org/doi/full/10.1164/rccm.200405-644ST
[3] Koenig, Steven M. and Jonathon D. Truwit. “Ventilator-Associated Pneumonia: Diagnosis, Treatment, and Prevention.” Clinical Microbiology Review. 2006 Oct; 19(4): 637–657. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1592694/
[4] Ding, Shifang et al. “Temporal Trends of Ventilator-Associated Pneumonia Incidence and the Effect of Implementing Health-care Bundles in a Suburban Community.” Chest. 2013 Nov; 144(5): 1461–1468. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3817928/#r1
[5] Improving Surveillance for Ventilator-Associated Events in Adults. Centers for Disease Control and Prevention (CDC). Mar, 2012. https://www.cdc.gov/nhsn/pdfs/vae/cdc_vae_communicationssummary-for-compliance_20120313.pdf
[6] Ventilator Associated Event (VAE). Center for Disease Control and Prevention (CDC). Jan 2018. https://www.cdc.gov/nhsn/pdfs/pscmanual/10-vae_final.pdf
[7] Kalanuria, Atul Ashok, Wendy Ziai, and Marek Mirski. “Ventilator-associated pneumonia in the ICU.” Critical Care. 2014; 18(2): 208. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4056625/
[8] Rea-Neto, Alvaro et al. “Diagnosis of ventilator-associated pneumonia: a systematic review of the literature.” Critical Care. 2008; 12(2): R56. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2447611/
[9] Amanullah, Shakeel MD. “Ventilator-Associated Pneumonia Overview of Nosocomial Pneumonias.” MedScape. Dec, 2015. https://emedicine.medscape.com/article/304836-overview
[10] Eliminating Serious, Preventable, and Costly Medical Errors – Never Events. Centers for Medicare and Medicaid Services (CMS). May 2006. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2006-Fact-sheets-items/2006-05-18.html
[11] CMS Improves Patient Safety for Medicare and Medicaid by Addressing Never Events. Centers for Medicare and Medicaid Services (CMS). Aug. 2008. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-Sheets/2008-Fact-Sheets-Items/2008-08-042.html
[12] Stone, Patricia W. et al. “CMS Changes in Reimbursement for HAIs–Setting A Research Agenda.” Medical Care. 2010 May; 48(5): 433–439. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2881841/
[13] Restrepo, Marcos I. et al. “Economic Burden of Ventilator-Associated Pneumonia Based on Total Resource Utilization.” Infection Control and Hospital Epidemiology. 2010; 31(5):509-515.
[14] Talbot, Thomas R. et al. “Sustained Reduction of Ventilator-Associated Pneumonia Rates Using Real-Time Course Correction With a Ventilator Bundle Compliance Dashboard.” Infection Control & Hospital Epidemiology. 2015;36(11):1261–1267
[15] Pogorzelska, Monika et al. “Impact of the ventilator bundle on ventilator-associated pneumonia in intensive care unit.” International Journal for Quality in Health Care, Volume 23, Issue 5, 1 October 2011; 538–544. https://academic.oup.com/intqhc/article/23/5/538/1866400
This webpage contains links to third party abstracts and/or publications. With respect to those materials, please note that Vapotherm’s Hi-VNI® technology is a tool for treating the signs and symptoms of respiratory distress in patients for whom prescribers desire to add heat and moisture to breathing gases. The linked materials may describe certain outcomes in relation to the use of Vapotherm’s Hi-VNI Technology, but individual results may vary. Practitioners should refer to the full indications for use and operating instructions of any products referenced herein before prescribing them.