Use of High Velocity Nasal Insufflation in combination with servo controlled FiO2 delivery for the ambulation of a patient with severe Interstitial Lung Disease (ILD)
Thomas Hillmann, Respiratory Physiotherapist
University of Essen, Ruhrlandklinik
Vapotherm’s high velocity therapy is a tool for treating respiratory distress. Although individual results may vary, Vapotherm believes this case study is an example of the clinical benefit Vapotherm’s high velocity therapy can have on patient ambulation . Practitioners should refer to the full indications for use and operating instructions of any products referenced herein before prescribing them.
Introduction
Ambulation, mobilization and training area crucial part within the management of severely dyspneic patients awaiting lung transplant.
A good physical status increases the probability of a positive outcome after transplant surgery[1]. Physical activity reduces the incidence of infections while on the waitlist and also has impactful positive effects on mental health and quality of life[2]. Our main therapeutic pillars for patients awaiting transplant are symptom control (dyspnea as the main symptom), avoidance of infections and complications, and physical training for which offloading work of breathing is essential.
Patient History and Presentation
We are reporting on a 36 year-old female patient hospitalized at our specialized Transplant Unit at the University of Essen, Germany. The patient was admitted from a secondary hospital due to a deterioration of her underlying Idiopathic Pulmonary Fibrosis (IPF). She has been listed for transplantation at EuroTransplant since March 2020. Her symptoms included increasing dyspnea at rest and inability to walk or exercise. At an O2-delivery of 8 L/min, she was suffering from Speech-related dyspnea and was severely compromised in her activities of daily life.

Treatment and Response
Initially, the patient received a steroid bolus which seemed to be beneficial at least in her perception.
In terms of respiratory support, we decided to switch the severely dyspneic patient from 8-12 L/min low flow oxygen (LFO2) onto Vapotherm’s high velocity therapy at 20 L/min of flow. The FiO2 was adjusted automatically by the Vapotherm Oxygen Assist Module* and varied when resting between 50 and 90% FiO2 based on a target SpO2 of 93% when resting. Although the patient disliked the sound of this high velocity device, she ultimately adopted the therapy as she immediately felt the relief in speech-related dyspnea.
We decided to start her on an individualized ambulation program which we kicked off with a 6-minute walk test (6-MWT) to compare the distance and dyspnea score to a 6-MWT she completed 48 hours prior.
Her walking distance with 10 l/min low flow oxygen was 90m with a mean pace of 0.25m/sec. On the BORG Dyspnea Scale she declared a level of 3/10 at start of the test and a level of 8/10 one minute after concluding the 6-MWT.
| Low Flow Oxygen | HVNI & OAM | |
|---|---|---|
| Support | nasal cannula 10 liters per Minute | HVNI 30LPM FiO2 60-100% |
| BORG after 6-MWT (BORG prior to 6-MWT) | 8/10 (3/10) | 3/10 (2/10) |
| Walking distance | 90m | 195m |
| Mean pace | 0,25 m/sec | 0,54m/sec |
Table 1: 6-MWT outcomes Low Flow versus high velocity therapy & OAM
On 30 L/min of High Velocity Nasal Insufflation (HVNI) delivered via Vapotherm’s Transfer Unit (VTU) in combination with OAM, her walking distance was 195m with a mean pace of 0.54m/sec (see Table 1).
Her FiO2 varied in between 60 and 100%, which resulted in a mean SpO2 of 94% ranging from 91 to 100% (See Figure 2). Also, her dyspnea score at the end of the exercise was dramatically reduced. Before starting she declared a level of 2/10 and after completing the distance, she went up to only 3/10 (See Table 1). All clinical treatments and conditions beside the technology for oxygen delivery and titration were comparable. Same Staff assisted at same time of the day with comparable BORG-Dyspnea-Score at beginning of the exercise.

Discussion
High Velocity Nasal Insufflation seems to have effectively supported this patient’s work of breathing both while at rest as well as while exercising. The Oxygen Assist Module in conjunction with the VTU allowed the patient to focus on the ambulation rather than on respiratory issues. This had an impact on both the patient as well as the physiotherapist who was able to focus on the ambulation and did not have to adjust oxygen delivery according to the SpO2 as the OAM quickly and effectively facilitated this task.
We frequently see patients experiencing an increase in dyspnea and severe desaturation after exercising is completed. This is impressively documented by the OAM Graph in Figure 2. After exercise ends at 10:42 the patient first calms down but then the O2 demand increases again (green line). OAM was effectively able to avoid this turning into hypoxia and dyspnea (blue line).
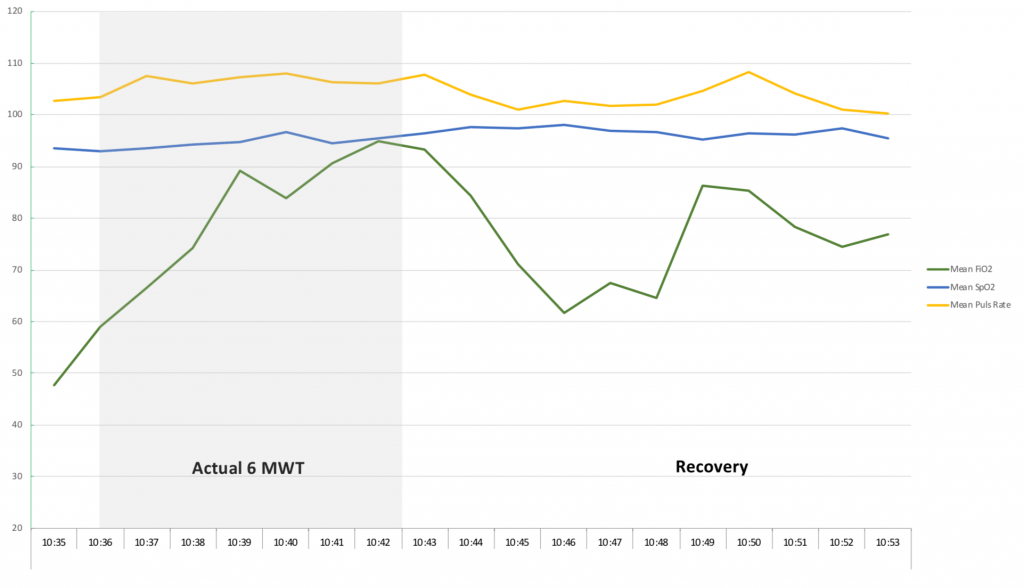
Figure 2: OAM Graph: SpO2 versus FiO2 and PR
Conclusion
The use of HVNI in concert with the servo control of OAM resulted in a great improvement in the patient’s dyspnea during the course of ambulation. This course of treatment is believed to be a significant benefit in this patient’s care as she awaits lung transplant.
* The Oxygen Assist Module (OAM) is not yet available in all regions.
REFERENCES
[1] Melinda LI: Pulmonary rehabilitation in lung transplant candidates; Journal for Heart and Lung Transplant 2013; http://dx.doi.org/10.1016/j.healun.2013.04.002
[2] Carolyn L. Rochester: Pulmonary Rehabilitation for Respiratory Disorders Other than Chronic Obstructive Pulmonary Disease; Clin Chest Med 35 (2014) 369–389; http://dx.doi.org/10.1016/j.ccm.2014.02.016
ADDITIONAL REFERENCES
Daniel Langer : Rehabilitation in Patients before and after Lung Transplantation; Respiration 2015; DOI: 10.1159/000430451
Carolyn L. Rochester: Pulmonary Rehabilitation for Patients Who Undergo Lung-Volume-Reduction: Respiratory Care 2008; Vol 53 No 9
Mariana Hoffmann: Effects of pulmonary rehabilitation in lung transplant candidates: a systematic review; BMJ Open 2017;7:e013445. doi:10.1136/bmjopen-2016- 013445
American Thoracic Society: https://www.thoracic.org/patients/patient-resources/resources/pulmonary-exercise-training-transplantation.pdf