How does Vapotherm High Velocity Therapy Compare to Noninvasive Positive Pressure Ventilation (NiPPV)?
Vapotherm high velocity therapy provides mask-free ventilatory support to patients in respiratory distress. Given the cannula interface, this modality often gets confused for generic high flow—a respiratory support tool with a cannula interface that delivers high liters of flow at low velocity. However, unlike generic high flow, high velocity therapy is indicated for ventilatory support and can be used as a frontline tool for respiratory failure in patient populations traditionally treated with NiPPV. But what patient types can be managed and how does this Mask-Free NIV® compare to traditional NIV when it comes to patient outcomes?
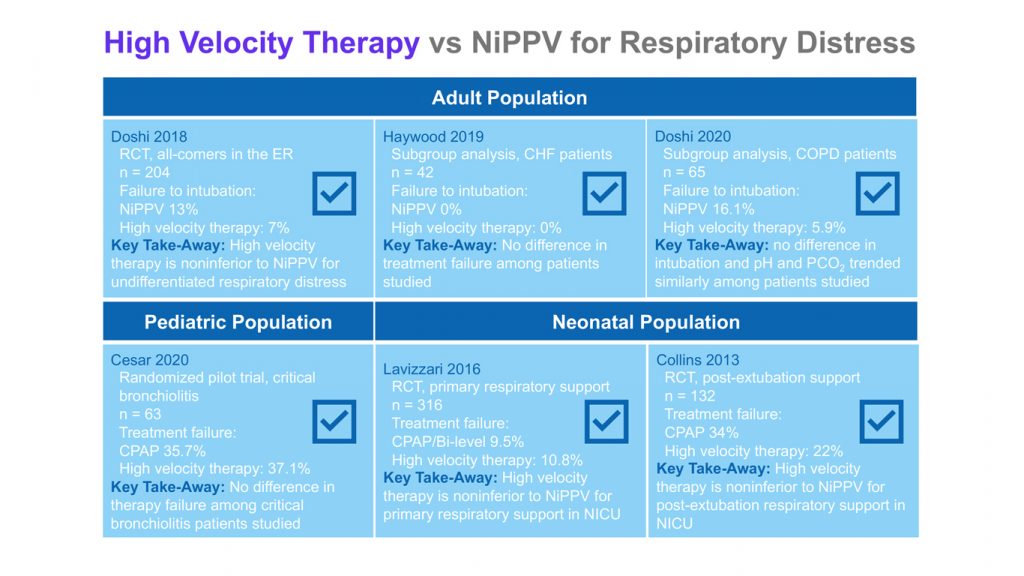
The figure below illustrates the summaries of studies examining comparisons between these two modalities.
The Adult Population
Adult All-Comers in the Emergency Department: Doshi and colleagues (2018) conducted a head-to-head randomized controlled trial comparing Vapotherm high velocity therapy and NiPPV in the treatment of emergency department patients with respiratory distress.1 Clinicians in the participating study centers randomized patients presenting in the emergency department with undifferentiated respiratory distress—i.e. the physicians included patients presenting with a variety of causes of their respiratory distress – including hypoxemic and hypercapnic respiratory failure —to either NiPPV or Vapotherm high velocity therapy.
The trial found no difference between the therapies in intubation rates or treatment failure rates. In other words, the patient outcomes regardless of whether patients were treated with the traditional modality of NiPPV or with high velocity therapy, were comparable. The authors concluded that Vapotherm high velocity therapy is noninferior to NIPPV for the treatment of adult patients experiencing undifferentiated respiratory failure in the Emergency Department.
Although there was similar efficacy between the two modalities, physicians rated high velocity therapy more favorably when it came to physician perception of patient response, patient comfort, and simplicity of use. [1]
For an in-depth summary of the Doshi 2018 trial, download this free eBook.
COPD Patients: Doshi and colleagues (2020) published a subgroup analysis of the above trial focused on just COPD patients and their outcomes.[2] Approximately one third of the patients in the trial — 65 out of 204 — had a discharge diagnosis that included hypercapnic respiratory failure or COPD and the question was how the these patients’ outcomes compared between Vapotherm high velocity therapy and NiPPV.
The authors found that, Vapotherm therapy had comparable outcomes to NiPPV in the treatment of respiratory distress among these COPD patients. You can read an in-depth summary of this analysis here.
CHF Patients: Similarly to the COPD subgroup analysis, Haywood and colleagues (2019) took the data from the large randomized controlled trial and analyzed it for the Congrative Heart Failure (CHF) patient population.[3] There was no difference in primary outcomes of intubation rate or therapy success between NiPPV and high velocity therapy among these patients. Additionally, there was no significant difference in baseline patient characteristics between the two randomized groups. You can read a more detailed summary of the study here.
Overall, these studies comparing NiPPV to high velocity therapy in adult patients suggest that physicians can use either modality for the management of respiratory distress.
The Pediatric Population
Bronchiolitis Patients: Cesar and colleagues (2020) conducted a pilot study comparing CPAP to Vapotherm high velocity therapy in infants with critical bronchiolitis.[4] The authors defined treatment failure as escalation to either intubation or bi-level NiPPV. In these patients studied, the two arms showed similar outcomes for both, treatment failure and PICU length of stay, as summarized here.
The Neonatal Population
Primary Respiratory Support: In a randomized controlled trial, Lavizzari and colleagues (2016) examined how Vapotherm high velocity therapy compares to CPAP/ bi-level PAP for RSD support in premature neonates.[5] They concluded that high velocity therapy was as effective as traditional NIV support in this patient population.
Post-Extubation Support: Collins and colleagues (2013) conducted a randomized controlled trial comparing Vapotherm high velocity therapy to CPAP for post-extubation support of premature neonates. Similar to Lavizzari’s outcomes, the authors found that high velocity therapy was noninferior to the traditional modality of CPAP.[6]
It’s important to note that both of these trials were conducted using exclusively Vapotherm high velocity therapy. These outcomes should not be conflated with similar trials that compare low-velocity high flow modalities to pressure-based NIV. Although generic high flow and high velocity both use nasal cannula interfaces, the two modalities are mechanistically different. This summary of ten studies in neonates illustrates some of the differences in patient outcomes between HFNC and high velocity/Mask-Free NIV.
One Comfortable and Effective Tool Across Patient Populations
In conclusion, studies that examine how high velocity therapy compares to mask-based NIV—like CPAP or bi-level PAP—have shown similar patient outcomes in the management of respiratory distress. This suggests that Mask-Free NIV can be an attractive alternative to traditional NIV modes, giving clinicians an efficacious, comfortable, and safe tool in their arsenal.
Download your free eBook on high velocity therapy and COPD.
REFERENCES
[1] Doshi, Pratik et al. High-Velocity Nasal Insufflation in the Treatment of Respiratory Failure: A Randomized Clinical Trial. Annals of Emergency Medicine, 2018.
[2] Doshi P, Whittle JS, Dungan G et al, The ventilatory effect of high velocity nasal insufflation compared to noninvasive positive-pressure ventilation in the treatment of hypercapneic respiratory failure: A subgroup analysisLung. 2020 Apr 6. https://doi.org/10.1016/j.hrtlng.2020.03.008
[3] Haywood ST, Whittle JS, Volakis LI et a HVNI vs NiPPV in the Treatment of ADHF: Subgroup analysis of a multi-center trial in the ED. American Journal of Emergency Medicine, 2019.
[4] Cesar, Regina Grigolli, Bibiane Ramos Pinheiro Bispo, Priscilla Helena Costa Alves Felix, Maria Carolina Caparica Modolo, Andreia Aparecida Freitas Souza, Nelson K. Horigoshi, Alexandre T. Rotta.High-Flow Nasal Cannula versus Continuous Positive Airway Pressure in Critical Bronchiolitis: A Randomized Controlled Pilot. J Pediatr Intensive Care. April 2020. DOI: 10.1055/s-0040-1709656
[5] Lavizzari A, Colnaghi M, Ciuffini F, Veneroni C, Musumeci S, Cortinovis I, Mosca F. “Heated, humidified high-flow nasal cannula vs nasal continuous positive airway pressure for respiratory distress syndrome of prematurity – a randomized clinical noninferiority trial.” JAMA Pediatr. 2016 Aug 8.
[6] Collins C, Holberton J, Barfield C, Davis P. “A randomized controlled trial to compare heated humidified high-flow nasal cannulae with nasal continuous positive airway pressure postextubation in premature infants.” J Pediatrics. 2013 May; 162: 949-54.